As individual responsibility for healthcare costs grows, brokers are increasingly critical to the proliferation and ultimate success of consumer-driven health plan benefits. In turn, their knowledge is key to the consumer’s ability to comprehend and fully realize the value of CDHPs. However, benefits tech firm Alegeus’ 2017 Broker and Employer CDH Insights Report identifies knowledge gaps over CDH benefits.
Of the 502 U.S.-based benefit brokers surveyed, 68% perceive themselves to be highly fluent in CDH benefits. But, other findings in the study indicate these brokers might mistake over-confidence for fluency.
Only 39% of brokers said they received advanced training in the form of consultative techniques. John Young, senior vice president of consumerism and strategy at Alegeus, says advanced training can consist of product capabilities, plan design, specifics on statutory regulations when it comes to health savings accounts and best practices for introducing a consumer-driven strategy for the first time.
“Basic training might be account features and concepts such as ‘HSAs are owned by the individual and the health reimbursement arrangement is generally owned by the employer,’” Young says. “Advanced training needs to go beyond all of that.”
Room for improvement
When asked to self-rate their understanding of specific CDH benefit concepts, brokers said their level of knowledge with regard to wellness plan incentives can improve. There are many different types of wellness programs, Young points out, which can make it difficult to incentivize each individual plan and keep track of the process.
Scott Wood, principal and CEO of Benefit Commerce Group out of Scottsdale, Ariz., agrees with Young that identifying where to place incentives and how to track ROI can be difficult. “We have tools, systems and analytics where we can get granular data from health plans and track experience, utilization, gaps in care and future medical risk,” Wood says. “With that data, you get a better handle on the ROI and what appropriate incentives can be distributed.”
30 leaders whose unique client management strategies, innovative data manipulation and other industry-leading skills are transforming the field
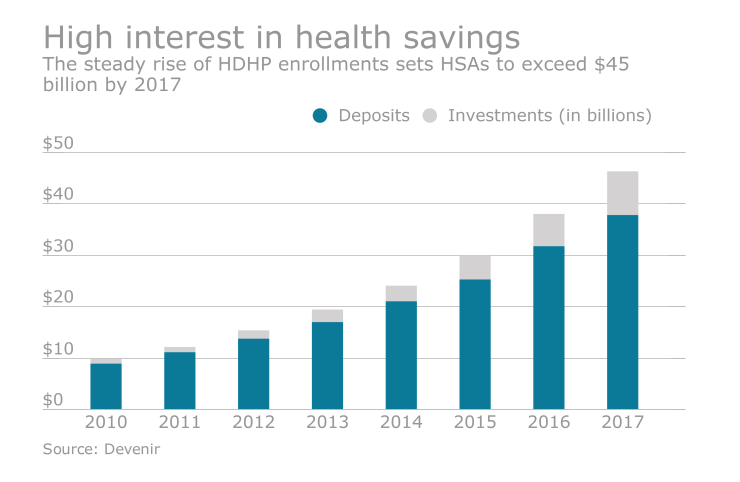
Additionally, 30% of brokers rated their aptitude as average or below average when discussing market trends related to account-based products such as an HRA, as well as encouraging employers to choose an HDHP coupled with an account over a more traditional health insurance offering, according to the Alegeus report.
“There’s a lot of misunderstanding that is created for brokers because health underwriters and actuaries have a lot of different views on pricing,” Wood says. “Also, there is the common myth that moving to a high deductible plan with an account is a reduction in benefits or a cost shift to employees.”
Young says there is a lot of market trend data showing otherwise, but because it is often sponsored by competing brokers, advisers can be hesitant to relay it.






